What is Endometriosis?
The American Congress of Obstetricians and Gynecologists defines endometriosis as a condition in which the type of tissue normally found on the inside lining of the uterus (the endometrium) is found outside the uterus. Endometriosis can affect a woman from the time of her first period to menopause. Sometimes, the disease can even last after menopause. At Woodlands OBGYN, our goal is to keep patients informed about endometriosis in efforts to help them maintain overall health and well-being.
Addressing Your Concerns
Endometriosis most commonly involves the uterus, ovaries, the small bowel, and the tissue lining the pelvis. Endometrial tissue acts just like the normal uterine lining in that it thickens, breaks down, and sheds or bleeds with each menstrual cycle.
However, because the displaced tissue has no way to exit the pelvic cavity, it becomes trapped and can cause pain, scar tissue, and adhesions. As a result, fertility problems may arise. Effective treatments are available.
What are the symptoms of endometriosis?
The primary symptom of endometriosis is pain, mostly in the lower abdomen, lower back, and pelvic area. Pain associated with endometriosis is usually in tandem with a woman’s monthly menstrual cycle, but in more severe cases, can occur more frequently. The amount of pain a woman feels is not linked to how much endometriosis she has. Some women have no pain even though their disease affects large areas, or there is scarring. Some women, on the other hand, have severe pain even though they have only a few small areas of endometriosis.
General symptoms of endometriosis can include, but are not limited to:
- Painful (or disabling) menstrual cramps; pain may worsen over time
- Chronic pelvic pain (includes lower back pain and pelvic pain)
- Pain during or after sex
- Intestinal pain
- Painful bowel movements or painful urination
- Heavy menstrual periods
- Spotting or bleeding between periods
- Infertility
- Gastrointestinal symptoms that are like those of a bowel disorder
- Fatigue
How do I know if I have endometriosis?
If you think you might have endometriosis, talk with your Woodlands OBGYN physician. There are a number of tests we can perform to determine if you have endometriosis.
The only way to know for sure if you have endometriosis is to have a laparoscopy. This is a surgical procedure performed under general anesthesia in which a camera is used to see inside your abdomen. Your surgeon can then check your organs to see if any growths or tissue from endometriosis exists. This procedure will show the location, extent, and size of the growths and begin treatment by removing endometriosis.
What causes endometriosis?
No one knows for sure what causes this disease. One theory is that during menstruation some of the menstrual tissue backs up through the fallopian tubes into the abdomen, where it implants and grows. Another theory suggests that endometriosis may be genetic or run in families.
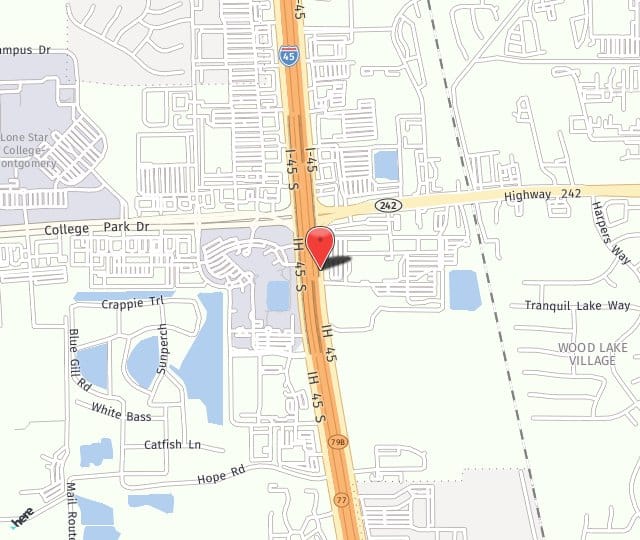
What is the treatment for endometriosis in The Woodlands, TX?
There is no cure for endometriosis, but there are many treatments, each of which has pros and cons. It is important to build a good relationship with your doctor, so you can decide what option is best for you.
Schedule a Woodlands, TX Endometriosis Consultation
To schedule an appointment, call us today at 281.364.9898